Case Presentation:
Trigeminal Neuralgia & Microvascular Decompression - Case 2
History & Physical
- 77-year-old right-handed gentleman, who experienced a sharp lancinating pain in the right frontal scalp region approximately four months prior to presentation. This pain would radiate from the right frontal scalp (V1 distribution) to the right brow, as well as the right temporal region. He experienced anywhere from six to seven of these pain episodes a day, each one lasting a couple of seconds. The intensity of the pain at onset was 10/10 on visual analog scale. There were no triggering stimuli that initiated these pain episodes.
- On examination, the patient had no neurological deficit with the exception of diminished sensitivity to cold, heat, or touch in this region.
- He was diagnosed with typical trigeminal neuralgia.
Imaging

MRI scan of his brain demonstrated a vascular structure impinging and compressing the trigeminal nerve at root entry zone on the right.
Surgical Procedure
- Having been correctly diagnosed with trigeminal neuralgia, and been refractory to proper medical management, he underwent microvascular decompression of the trigeminal nerve by a right retrosigmoid craniectomy with intraoperative neurophysiological monitoring and stereotactic computer aided navigation.
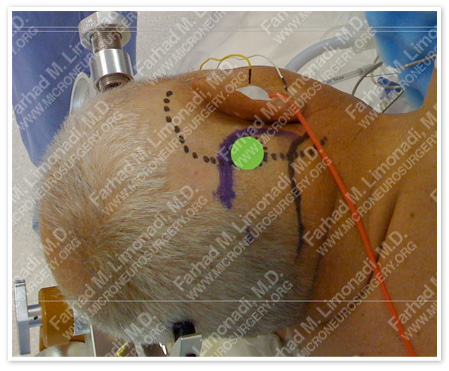
The planned bony exposure is marked in green (circle), and important vascular and bony landmarks (mastoid tip, transverse and sigmoid sinuses) are also marked.
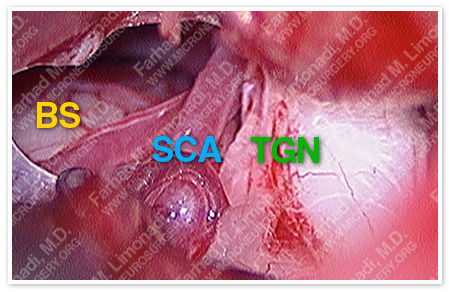
Trigeminal nerve (TGN) is distorted and compressed by a pulsating superior cerebellar artery (SCA) and its. Brain stem is also marked (BS).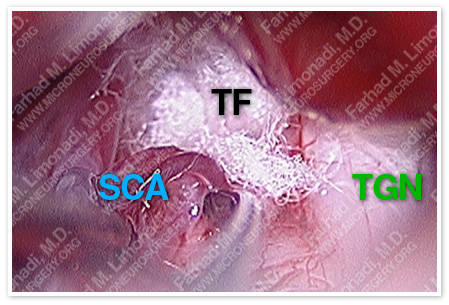
Superior cerebellar artery (SCA) has been mobilized from its constrained position at root entry zone of trigeminal nerve (TGN) and maintained separated by a teflon felt (TF) positioned between the two.
Post-op Course
- Patient did well postoperatively with complete resolution of his facial pain. He was discharged from the hospital and returned to full function.